 The pace of antibody therapeutics development accelerated in 2017, and this faster pace is projected to continue through 2018. Notably, the annual number of antibody therapeutics granted a first approval in either the European Union (EU) or United States (US) reached double-digits (total of 10) for the first time in 2017. The 10 antibodies granted approvals are: brodalumab, dupilumab, sarilumab, guselkumab, benralizumab, ocrelizumab, inotuzumab ozogamicin, avelumab, duvalumab, and emicizumab. Brodalumab, however, had already been approved in Japan in 2016.
The pace of antibody therapeutics development accelerated in 2017, and this faster pace is projected to continue through 2018. Notably, the annual number of antibody therapeutics granted a first approval in either the European Union (EU) or United States (US) reached double-digits (total of 10) for the first time in 2017. The 10 antibodies granted approvals are: brodalumab, dupilumab, sarilumab, guselkumab, benralizumab, ocrelizumab, inotuzumab ozogamicin, avelumab, duvalumab, and emicizumab. Brodalumab, however, had already been approved in Japan in 2016.
As of mid-December 2017, 10 antibody therapeutics (ibalizumab, burosumab, tildrakizumab, caplacizumab, erenumab, fremanezumab, galcanezumab, romosozumab, mogamulizumab, cemiplimab) were in regulatory review in the EU or US, and regulatory actions on their marketing applications are expected by the end of 2018.
Based on company announcements and estimated clinical study primary completion dates, and assuming the study results are positive, marketing applications for at least 13 antibody therapeutics that are now being evaluated in late-stage clinical studies may be submitted by the end of 2018. Of the 13 candidates, 8 are for non-cancer indications (lanadelumab, crizanlizumab, ravulizumab, eptinezumab, risankizumab, satralizumab, brolucizumab, PRO140) and 5 are for cancer (sacituzumab govitecan, moxetumomab pasudotox, cemiplimab, ublituximab, isatuximab).
Additional antibody therapeutics to watch in 2018 include 19 mAbs undergoing evaluation in late-stage studies with primary completion dates in late 2017 or during 2018. Of these mAbs, 9 are for non-cancer indications (lampalizumab, roledumab, emapalumab, fasinumab, tanezumab, etrolizumab, NEOD001, gantenerumab, anifrolumab) and 10 are for cancer indications (tremelimumab, isatuximab, BCD-100, carotuximab, camrelizumab, IBI308, glembatumumab vedotin, mirvetuximab soravtansine, oportuzumab monatox, L19IL2/L19TNF). Positive clinical study results may enable marketing application submissions in 2018. Brief summaries of these antibody therapeutics are provided in the ‘Antibodies to watch in 2018’ article, which is now available on the mAbs website. A PDF of this open-access article is available here.
Antibodies to watch in 2016: Mid-year update
 Since 2010, the “Antibodies to watch” article series has documented annually the number and identities of commercially sponsored antibody therapeutics in Phase 3 studies, regulatory review and those recently approved in the US and EU. Taken together, the articles have captured the extraordinary doubling of the number of antibody therapeutics in Phase 3 studies from 26 to 53, as identified in the “Antibodies to watch in 2010” and “Antibodies to watch in 2016” articles, respectively. Due to the highly dynamic nature of antibody therapeutics development, numerous transitions have occurred during 2016, and the Society offers here a mid-year update to data reported in the “Antibodies to watch in 2016” article.
Since 2010, the “Antibodies to watch” article series has documented annually the number and identities of commercially sponsored antibody therapeutics in Phase 3 studies, regulatory review and those recently approved in the US and EU. Taken together, the articles have captured the extraordinary doubling of the number of antibody therapeutics in Phase 3 studies from 26 to 53, as identified in the “Antibodies to watch in 2010” and “Antibodies to watch in 2016” articles, respectively. Due to the highly dynamic nature of antibody therapeutics development, numerous transitions have occurred during 2016, and the Society offers here a mid-year update to data reported in the “Antibodies to watch in 2016” article.
As described in our previous posts, 4 antibody therapeutics (atezolizumab, reslizumab, ixekizumab, obiltoxaximab) were granted first marketing authorizations in either the US or EU during January to June 2016. As of mid-2016, marketing applications for 8 antibody therapeutics are being considered for first approvals in the US or EU. Of these, 5 applications (olaratuzumab, bezlotoxumab, sarilumab, brodalumab, ocrelizumab) have Food and Drug Administration action dates during September -December 2016. Recommendations by the European Medicines Agency on applications for Xilonix and inotuzumab ozogamicin could be made in 2016, but additional time would be needed for the European Commission’s decision regarding whether to grant the marketing authorization. It thus remains to be seen whether the number of antibody therapeutics approved in the US or EU during 2016 will match or exceed the record of 9 approvals granted in a single year set in 2015.
As of mid-2016, 53 unique antibody therapeutics were in Phase 3 studies. This is the same total number noted in the “Antibodies to watch in 2016” article, but the antibodies included in the totals are not all the same. The tables included in this mid-year update result from the addition of antibodies that started a first Phase 3 study in late 2015 to mid-2016, and deletion of antibodies that transitioned to regulatory review, reverted to an earlier clinical phase or had their development suspended or terminated. Compared to the totals included in the “Antibodies to watch in 2016” article, the number of antibodies in Phase 3 studies for cancer indications as of mid-2016 decreased slightly (from 17 to 15, respectively), while those for non-cancer indications increased slightly (from 36 to 38, respectively).
Antibodies for cancer represent only 28% of the current commercial Phase 3 pipeline, although they are ~55% of the overall clinical pipeline of therapeutic antibodies. The 15 antibody therapeutics in Phase 3 studies for cancer indications are notable for the diversity in their composition. Of the 15, 6 (40%) are non-canonical antibodies (1 radiolabeled antibody, 1 scFv-containing liposome, 2 immunotoxins, 2 antibody-drug conjugates (ADCs)), and a majority of the canonical antibodies (i.e., full-length IgG1, 2 or 4) are Fc- or glyco-engineered to enhance functionality. The 2 ADCs now in Phase 3 studies represent a vanguard, as this type of antibody therapeutic has entered clinical studies in large numbers only recently. Of the ADCs currently in clinical studies, most (44/56, 79%) are in either Phase 1 or Phase 1/2 studies, and most (55/56) are for cancer indications. ADCs now comprise ~20% of the clinical pipeline of antibodies for cancer, but ~11% of all antibodies in clinical development. There is substantial diversity of the targets, drugs, linkers, and drug-to-antibody ratios of the ADCs in the clinic. For example, of the ADCs in the clinic, targets for 51 have been disclosed, and 39 of these 51 targets are unique, i.e., only one ADC in clinical studies is known to target that particular antigen. Antigens known to be the target of more than one ADC in clinical studies include CD19, CD37, EGFR, HER2 and mesothelin. The diversity of the molecules may initially serve as a hindrance, but knowledge gained by the development of this class of molecules should increase overall as more ADCs enter clinical studies, transition through the phases and join the two ADCs currently on the market, brentuximab vedotin (Adcetris®) and ado-trastuzumab vedotin (Kadcyla®).
Antibodies for non-cancer indications dominate the current commercial Phase 3 pipeline. Unlike the antibodies for cancer, the 38 antibodies in Phase 3 studies for non-cancer indications are mostly canonical full-length IgG1, 2 or 4 molecules. Only 4 of the 38 (~11%) are non-canonical molecules: 1 bispecific antibody and 3 antibody ‘fragments’ (scFv, Fab, nanobody). Like ADCs, bispecific antibodies are expected to comprise a larger percentage of the Phase 3 pipeline in the next ~6-8 years. Bispecific antibodies now comprise ~9% of the entire commercial pipeline of antibody therapeutics, but most (32/45, 71%) of those are currently in early clinical studies (either Phase 1 or Phase 1/2). Compared to ADCs, bispecific antibodies are undergoing evaluation in a broader range of indications, although the majority of bispecifics (30/45, 67%) are for cancer and they comprise ~11% of the clinical pipeline of antibodies for cancer. The two bispecific antibodies now on the market, catumaxomab (Removab®) and blinatumomab (BLINCYTO®), are both for cancer. Nevertheless, the one bispecific antibody now in Phase 3 studies, emicizumab, is for a non-cancer indication (hemophilia A).
The clinical pipeline of antibody therapeutics, including at Phase 3, is highly dynamic. The Antibody Society will continue to track antibodies in the clinic, and report progress to its members.
Acknowledgements: The Antibody Society thanks Hanson Wade for access to the Beacon ADC database.
Like this post? Please become a member!
Antibody Drug Conjugates – News
 Immunomedics announced the issuance of a novel patent (U.S. Patent 9,375,489) related to the company’s lead cancer therapeutic, sacituzumab govitecan, also known as IMMU-132. This antibody-drug conjugate (ADC) comprises a humanized antibody to the cancer target Trop-2 and is conjugated with SN-38, an active metabolite of the anti-cancer drug irinotecan. The patent entitled “Antibody-SN-38 Immunoconjugates with a CL2A Linker.” is the 28th issued U.S. patent covering the uses and composition of sacituzumab govitecan.
Immunomedics announced the issuance of a novel patent (U.S. Patent 9,375,489) related to the company’s lead cancer therapeutic, sacituzumab govitecan, also known as IMMU-132. This antibody-drug conjugate (ADC) comprises a humanized antibody to the cancer target Trop-2 and is conjugated with SN-38, an active metabolite of the anti-cancer drug irinotecan. The patent entitled “Antibody-SN-38 Immunoconjugates with a CL2A Linker.” is the 28th issued U.S. patent covering the uses and composition of sacituzumab govitecan.
The ADC is in development for the treatment of patients with many diverse solid cancers. The most advanced indication in development is triple-negative breast cancer (TNBC). Phase II are also studies ongoing in patients with metastatic non-small-cell lung cancer (NSCLC), small-cell lung cancer (SCLC) and in patients with metastatic urothelial cancers. According to Immunomedics’ updated clinical development plan for sacituzumab govitecan, in Q3 of 2016 the company plans to complete enrollment of additional patients into the ongoing single-arm Phase II study for patients with relapsed/refractory metastatic TNBC who received at least 2 prior therapies, including taxane. Immunomedics is collaborating with the FDA for completion of the ongoing Phase II trial and for submitting an Accelerated Approval registration application. Also discussions with the European Medicine Agency (EMA) have been initialized, and EMA has provided the company with advice on the scheduled Phase III trial.
In other news, AbbVie announced safety and preliminary efficacy data from a Phase I study of ABT-414. ABT-414 is an investigational ADC for treatment of epidermal growth factor receptor (EGFR) amplified, recurrent glioblastoma (GBM). Glioblastoma is the most common and most aggressive type of malignant primary brain tumor and in most cases a fatal disease. Amplified EGFR is the most common genetic mutation associated (~50% are EGFR mutations) with malignant GBM. With standard of care therapy, patients with GBM have a median survival of 15 months after diagnosis and two-year survival is 30%, demonstrating the urgent unmet need for new treatment options.
Published data showed no dose-limiting toxicities and frequent, reversible ocular toxicities. Furthermore, an estimated 30% (n=44) of patients treated with ABT-414 as monotherapy were progression free at six months [95% CI=17, 44] (secondary endpoint). Best Response Assessment in Neuro-Oncology (RANO) Criteria identified two partial responses, 18 patients with stable disease, and 24 with progressive disease for a total of 44 patients with complete data.
The most common serious adverse event (>1 patient) (n=48) was seizure (8%) as of January 7, 2016. Grade 3/4 treatment emergent adverse events (TEAEs) (>1 patient) were keratitis (15%), corneal epithelial microcysts (8%), hemiparesis (6%), hyperglycemia (6%), muscular weakness (6%), seizure (6%), blurred vision (4%) and ulcerative keratitis (4%).The most common TEAEs (≥25% patients) in this study arm were blurred vision (60%), headache (29%), photophobia (29%), dry eye (27%), eye pain (27%), and fatigue (27%).
Using bispecific antibodies for T-cell recruitment
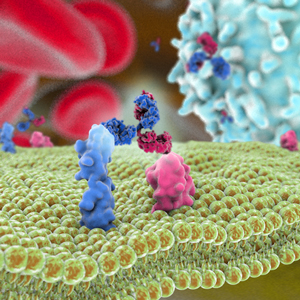
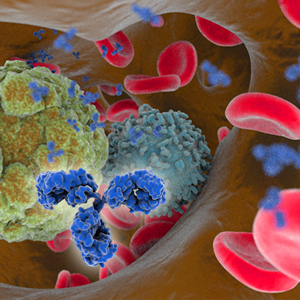
T-cell recruitment for the treatment of cancer has garnered substantial interest over the past thirty years [1,2]. In this type of therapy, activated tumor-specific cytotoxic T-cell lymphocytes are directed to malignant tumor, and subsequently destroy them. Activation of this mechanism relies on T cells and tumor cells being in close proximity to one another. One popular strategy for bringing the cells together involves use of a bispecific antibody [3] where the dual-antigen specificity can enable simultaneous binding of a tumor-specific antigen along with an antigen present on a cytotoxic T-cell. In addition to having the advantage of enhanced functionality compared to a monospecific antibody, garnering dual specificity from single-agent therapy can simplify the development process, e.g., only one molecule needs to be approved. Two bispecific antibodies that take advantage of this principle have been approved: catumaxomab (Removab®) for the treatment of malignant ascites secondary to epithelial cancers and blinatumomab (Blincyto®) as second-line treatment for B cell acute lymphocytic leukemia (ALL).
Catumaxomab is a monoclonal IgG-like antibody [4]. It is termed trifunctional because one of the Fab arms binds epithelial tumor cells via the epithelial cell-adhesion molecule (EpCAM) antigen site, the other Fab arm binds cytotoxic T cells via the CD3 receptor, while the Fc acts as the third site of action, selectively engaging Fcγ receptor I-, IIa- or III on accessary cells. Thusly in this strategy, tumor cell destruction relies not only on T-cell lysis, but also on T-cell activation of accessory cells such as macrophages, dendritic cells and natural killer cells, which engage in destruction of tumor cells by various mechanisms such as perforin-mediated lysis, antibody-mediated phagocytosis and cytokine release. In 2009, catumaxomab became the first bispecific antibody to be approved, for use in Europe [4].
Blinatumomab, in contrast, is a bispecific T cell engager (BiTE) [5]. It is composed of two tandem single-chain variable fragments, each with unique specificity, fused together by a short flexible linker. One arm of this bispecific molecule binds CD3 on T cells while the other arm binds CD19, an antigen found on almost all B-lineage ALL cells and in many places throughout B cell differentiation. Bridging of the two antigens enables T-cell activation and exertion of cytotoxic activity by lysis of target B cells. Two advantages of this bispecific molecule are its small size, which results in fast systemic clearance and ensures close proximity of T cells to target cell, and its flexibility, which is thought to lead to efficient induction of T-cell activation by enabling optimal interaction with target epitopes on the two opposing cell membranes. In some cases, bifunctionality is preferred over trifunctionality because of concern that the Fc receptor interactions could potentially lead to dampening of the immune response. In 2014, blinatumomab became the first bispecific antibody approved for use in the United States. It is currently being evaluated in Phase 2 clinical trials for the treatment of other ALL-related diseases [6].
Nonetheless despite very encouraging preclinical results [7-9] and extensive clinical activities [10-13], additional successful outcomes in the clinic have not been forthcoming. Of the twenty novel bispecific antibodies that entered first-in-humans clinical studies in 2014-2015, approximately half invoke a T-cell recruiting mechanism. Despite this abundance, none of these have advanced beyond Phase 1. Thus far, toxicity and lack of significant anti-tumor response appear to be the primary barriers to advancement of these agents. Improving the selectivity of T-cell activation is being examined as a way to address toxicity issues. To increase the effectiveness of the agents, alternate dose administration strategies are being tested. For example, blinatumomab’s dosing was changed to continuous infusion instead of intravenous injection to ensure continuous activation of T cells against target cells [14]. In addition, use of T-cell recruiting bispecific antibodies as first in-line treatment or as a component of combination therapies are also being evaluated to determine whether significant gains in patient response can be achieved. If such gains can be achieved with these approaches, more T-cell activating bispecific antibodies that will successfully meet patient needs may be available in the future.
1. Staerz UD, Kanagawa O, Bevan M. Hybrid antibodies can target sites for attack by T cells. Nature 1985; 314:628–31.
2. Perez P, Hoffman RW, Shaw S, Bluestone JA, Segal DM. Specific targeting of cytotoxic T cells by anti-T3 linked to anti-target cell antibody. Nature 1985; 316:354–6.
3. Weidle UH, Kontermann RE, Brinkmann U. Tumor-antigen–binding bispecific antibodies for cancer treatment. Seminars in Oncology 2014; 41:653–60.
4. Linke R, Klein A, Seimetz D. Catumaxomab: Clinical development and future directions. mAbs 2014; 2:129–36.
5. Wolf E, Hofmeister R, Kufer P, Schlereth B, Baeuerle PA. BiTEs: bispecific antibody constructs with unique anti-tumor activity. Drug Discovery Today 2005; 10:1237–44.
6. Turner J, Schneider S. Blinatumomab: A new treatment for adults with relapsed acute lymphocytic leukemia. Clin J Oncol Nurs. 2016; 20:165–8.
7. Deo YM, Sundarapandiyan K, Keler T, Wallace PK, Graziano RF. Bispecific molecules directed to the Fc receptor for IgA (FcαRI, CD89) and tumor antigens efficiently promote cell-mediated cytotoxicity of tumor targets in whole blood. J Immunol 1998; 160:1677–86.
8. Löffler A, Kufer P, Lutterbüse R, Zettl F, Daniel PT, Schwenkenbecher JM, Riethmüller G, Dörken B, Bargou RC. A recombinant bispecific single-chain antibody, CD19 x CD3, induces rapid and high lymphoma-directed cytotoxicity by unstimulated T lymphocytes. Blood 2000; 95:2098–103.
9. Heiss MM, Ströhlein MA, Jäger M, Kimmig R, Burges A, Schoberth A, Jauch K-W, Schildberg F-W, Lindhofer H. Immunotherapy of malignant ascites with trifunctional antibodies. Int J Cancer 2005; 117:435–43.
10. Begent RH, Verhaar MJ, Chester KA, Casey JL, Green AJ, Napier MP, Hope-Stone LD, Cushen N, Keep PA, Johnson CJ, et al. Clinical evidence of efficient tumor targeting based on single-chain Fv antibody selected from a combinatorial library. Nat Med 1996; 2:979–84.
11. Burges A, Wimberger P, Kümper C, Gorbounova V. Effective relief of malignant ascites in patients with advanced ovarian cancer by a trifunctional anti-EpCAM× anti-CD3 antibody: a phase I/II study. Clin Cancer Res. 2007; 13:3899-905.
12. De Gast GC, Van Houten AA, Haagen IA, Klein S, De Weger RA, Van Dijk A, Phillips J, Clark M, Bast BJ. Clinical experience with CD3 X CD19 bispecific antibodies in patients with B cell malignancies. J Hematother. 1995;4:433-7.
13. Heiss MM, Murawa P, Koralewski P, Kutarska E, Kolesnik OO, Ivanchenko VV, Dudnichenko AS, Aleknaviciene B, Razbadauskas A, Gore M, et al. The trifunctional antibody catumaxomab for the treatment of malignant ascites due to epithelial cancer: Results of a prospective randomized phase II/III trial. Int J Cancer 2010; 127:2209–21.
14. Klinger M, Brandl C, Zugmaier G, Hijazi Y, Bargou RC, Topp MS, Gökbuget N, Neumann S, Goebeler M, Viardot A, et al. Immunopharmacologic response of patients with B-lineage acute lymphoblastic leukemia to continuous infusion of T cell–engaging CD19/CD3-bispecific BiTE antibody blinatumomab. Blood 2012; 119:6226–33.
European Medicines Agency’s antibody PRIority MEdicines
 On June 1, the European Medicines Agency (EMA) announced that four medicines in development were accepted under their new PRIority MEdicines (PRIME) scheme, which focuses on medicines that may offer a major therapeutic advantage over existing treatments, or benefit patients without treatment options. In this voluntary scheme, EMA offers early, proactive and enhanced support to developers to optimize the generation of robust data on a medicine’s benefits and risks, and enable accelerated assessment of medicine applications. Early clinical data that shows a medicine has the potential to benefit patients with unmet medical needs must be provided for it to be accepted for PRIME access.
On June 1, the European Medicines Agency (EMA) announced that four medicines in development were accepted under their new PRIority MEdicines (PRIME) scheme, which focuses on medicines that may offer a major therapeutic advantage over existing treatments, or benefit patients without treatment options. In this voluntary scheme, EMA offers early, proactive and enhanced support to developers to optimize the generation of robust data on a medicine’s benefits and risks, and enable accelerated assessment of medicine applications. Early clinical data that shows a medicine has the potential to benefit patients with unmet medical needs must be provided for it to be accepted for PRIME access.
Of the four medicines given PRIME access to date, two, aducanumab and NI-0501, are antibody therapeutics. Aducanumab, which targets amyloid beta, has PRIME access as a treatment of Alzheimer’s disease. The antibody is currently being evaluated in two Phase 3 studies of patients with early Alzheimer’s disease. The primary objective of the studies is to evaluate the efficacy of monthly doses of aducanumab in slowing cognitive and functional impairment. An estimated 1350 patients will be enrolled in each study. Both studies were initiated in 2015, and have primary completion dates in February 2020.
NI-0501, a human mAb targeting interferon gamma, has PRIME access as a treatment of primary hemophagocytic lymphohistiocytosis (PHL). A Phase 2, open-label, single arm study to explore the safety, tolerability, pharmacokinetics and efficacy of intravenous multiple administrations of NI-0501 in children with PHL is currently recruiting patients. The study was initiated in 2013 and has an estimated enrollment of 10 patients. The primary completion date of the study is December 2016. NI-0501 has orphan drug designations in the European Union and United States. It also has the US Food and Drug Administration’s Breakthrough Therapy Designation, which, like the PRIME scheme, is intended to expedite the development and review of new therapies for serious or life threatening conditions that have shown encouraging early clinical results over available therapies.
Find information about the four medicines accepted under the PRIME scheme here.
Like this post? Please support the Society by registering here for a membership!